Non-Pharmaceutical Pain Management: Real Alternatives
When you hear "pain management," it’s easy to think of a prescription pad or the chemist's aisle. But what if you could manage discomfort without reaching for a pill? That’s exactly what non-pharmaceutical pain management is all about. It’s a hands-on approach using physical, psychological, and lifestyle-based strategies to get to the root of your pain, not just silence the symptoms.
It’s about empowering you to become an active participant in your own relief.
Rethinking Pain Relief Beyond the Pill Bottle
Relying solely on medication can sometimes feel like a temporary fix—a band-aid solution that depends entirely on the next dose. True, lasting comfort often comes from building a personal toolkit of strategies that work with your body to calm pain signals and build resilience. This is the heart of non-pharmaceutical pain management: a shift from passively receiving treatment to proactively taking back control.
This change in thinking is especially important here in Australia. While GPs are often our first port of call, their approach can be heavily weighted towards medication. In fact, an estimated 70% of GP visits for pain in Australia result in a medication prescription, often including opioids. This common practice doesn't always align with modern models of care that recommend drug-free therapies first, revealing a significant gap between advice and reality. You can find more details on this national approach from the Royal Australian College of General Practitioners.
This guide is designed to help you bridge that gap. We're not looking for a single magic bullet, because effective pain management is never that simple. Instead, we'll explore a combination of evidence-based methods you can tailor to your own body, needs, and lifestyle.
The Three Pillars of Drug-Free Pain Management
To make sense of all the options out there, it helps to group them into three core categories. Think of each one as a different pillar supporting your overall wellbeing, giving you different ways to influence pain signals and improve how you feel day-to-day.
These three pillars—Physical, Mind-Body, and Lifestyle—work together to form a complete, holistic strategy.
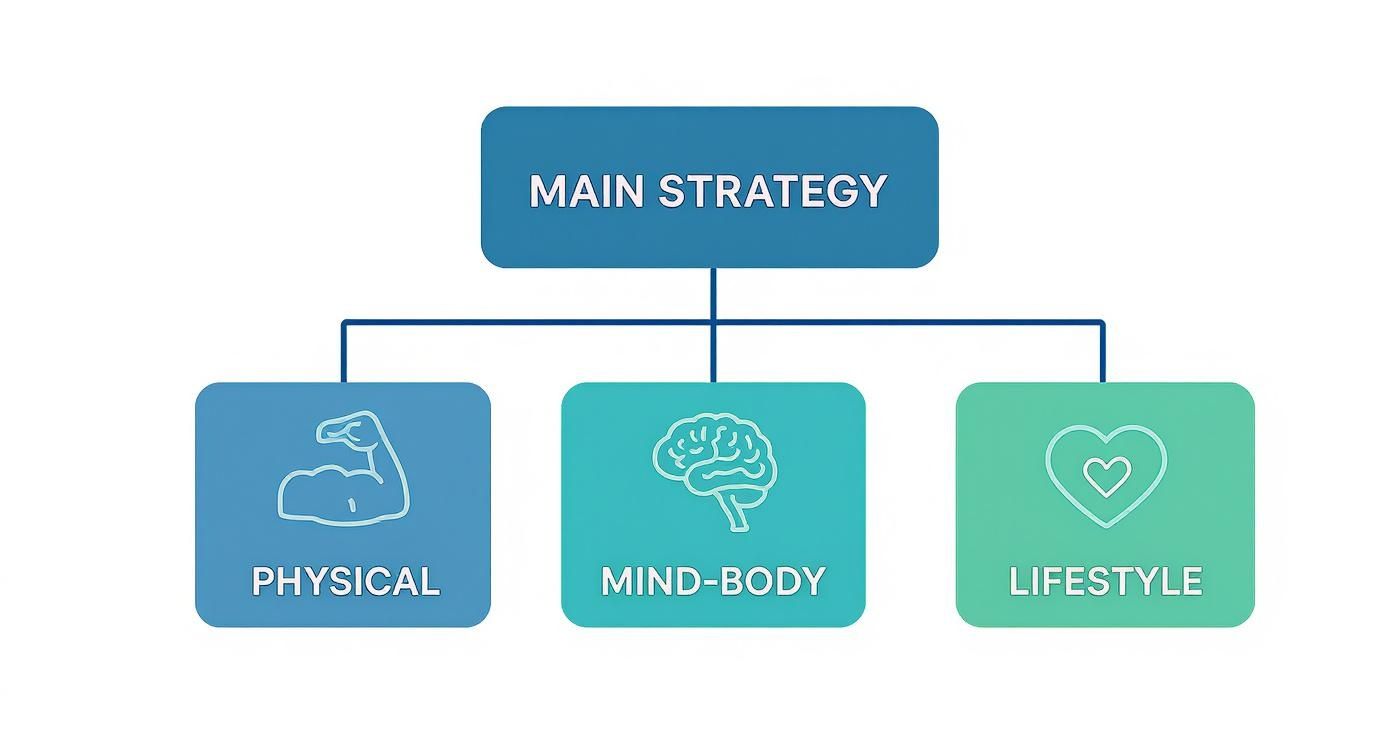
As the image shows, a truly solid plan isn't built on just one approach but on the combined strength of all three. By drawing from each category, you create a far more robust and adaptable toolkit for managing pain.
To get a clearer picture of what this looks like, let's break down the strategies we'll be exploring.
Your Non-Pharmaceutical Pain Management Toolkit
| Strategy Category | Primary Focus | Examples |
|---|---|---|
| Physical Therapies | Directly targeting the body to reduce pain signals and improve function. | Heat/cold packs, physical therapy, massage, TENS machines, acupuncture. |
| Mind-Body Techniques | Using the connection between your mind and body to change your perception of pain. | Relaxation exercises, mindfulness, meditation, Cognitive Behavioural Therapy (CBT). |
| Lifestyle Adjustments | Building a foundation of health that makes your body more resilient to pain. | Improving sleep hygiene, staying hydrated, gentle movement, ergonomic changes. |
This table serves as our roadmap. We’ll dive into each of these areas, giving you practical, evidence-based options to try.
The goal isn't just to stop feeling pain, but to build a life where pain has less power over you. It's about empowering yourself with knowledge and practical skills that you can use anytime, anywhere, without needing a prescription.
From simple therapies you can do at home to powerful techniques that reshape how your brain processes pain, you’re about to discover a world of effective alternatives. This is about moving beyond temporary fixes and building a lasting foundation for a more comfortable and active life.
Building Your Foundation with Physical Therapies
Physical therapies are often the bedrock of any solid, drug-free pain management plan. They offer direct, hands-on ways to soothe discomfort and, just as importantly, improve how your body actually works. These methods get right to the source of the pain, whether it’s knotted muscles, inflammation, or faulty movement patterns. Getting a handle on these techniques helps you build a strong foundation for real, lasting relief.
The easiest place to start is with hot and cold therapies—simple, surprisingly effective tools you can use right at home to tackle immediate pain. Think of them as two distinct tools for two very different jobs. They have opposite effects on blood flow, inflammation, and muscle tension, which makes them a versatile first line of defence against everyday aches.

Hot vs. Cold: When to Use Each Therapy
Knowing whether to reach for a heat pack or an ice pack is critical. It’s not just a matter of preference; grabbing the wrong one can sometimes make things worse. Understanding what each one does to your body is the key to getting it right.
Cold therapy, or cryotherapy, is your best friend for new injuries and inflammation. When you apply cold, it constricts your blood vessels. This simple action helps to:
-
Reduce swelling and fluid build-up around the injury.
-
Numb the local nerve endings, which provides that immediate sense of relief.
-
Slow down cellular metabolism, which can limit tissue damage in the moments after an injury.
It’s perfect for a freshly sprained ankle, a muscle strain after a workout, or the intense, throbbing pain that can come with some types of migraines. Applying a cold compress or a product like the Headache Cap to the forehead can effectively dull headache pain by calming inflamed blood vessels.
Heat therapy, on the other hand, is what you want for chronic muscle soreness, stiffness, and aches that aren't swollen. Heat does the exact opposite of cold—it dilates blood vessels. This:
-
Boosts blood flow, bringing more oxygen and nutrients to the area to help it heal.
-
Helps tight, spasming muscles to finally relax and eases up stiff joints.
-
Creates a comforting sensation that can reduce your overall perception of pain.
Think of using heat for a tension headache that stems from a stiff neck, a nagging lower back ache, or to warm up tight muscles before some gentle stretching. To explore this further, you can learn more about how heat therapy helps manage pain in our detailed guide.
A simple rule of thumb makes it easy: Ice for new injuries and inflammation, heat for old aches and stiffness. Trusting this basic principle helps you respond effectively to what your body is telling you.
Moving Beyond Basic Relief with Physiotherapy
While hot and cold packs are fantastic for short-term relief, they don't fix the underlying problem. That's where structured physiotherapy comes in. It’s a common myth that physio is just about stretching; in reality, it’s a highly personalised approach to pain management that focuses on restoring movement, building strength, and correcting the imbalances that caused the pain in the first place.
A good physiotherapist is a bit like a detective for your body. They’ll assess your specific situation to figure out why you’re in pain—is it poor posture from sitting at a desk, a muscle weakness that never healed properly, or a repetitive strain injury?
From there, they create a targeted program that’s far more than just a list of generic exercises. This professional guidance ensures that every movement has a purpose. It helps strengthen the muscles that support the injured area, improves your range of motion, and fundamentally retrains your body to move in a healthier, more efficient way.
By working with a professional, you don't just find temporary relief. You gain the knowledge and tools to stop the pain from coming back, putting you in long-term control of your physical wellbeing.
Tapping Into the Power of Your Mind-Body Connection
Pain isn’t just a physical signal. It's a complex experience, tangled up with our thoughts, emotions, and stress levels. This powerful link between what’s happening in our head and what we feel in our body is called the mind-body connection. Learning to tap into it is one of the most effective ways to manage pain without reaching for medication. It's about changing your relationship with pain from the inside out.
Instead of simply reacting to discomfort when it flares up, these techniques empower you to actively influence how your brain interprets pain signals. Think of it like adjusting the volume on a stereo – the music is still playing, but you can turn it down so it’s not blasting and overwhelming everything else. The goal isn't to pretend the pain doesn't exist, but to stop it from hijacking your focus and running your life.

Rewriting Your Pain Script with CBT
One of the most well-researched mind-body approaches is Cognitive Behavioural Therapy (CBT). It’s a practical, hands-on therapy that teaches you to spot and reframe the unhelpful thought patterns and behaviours that often come with chronic pain. The core idea is simple: our thoughts, feelings, and physical sensations are all linked.
For someone living with chronic headaches, a common negative thought pattern is "catastrophising". This is where your mind immediately jumps to the worst possible outcome. A slight throb behind the eyes might trigger a cascade of thoughts like, "Here we go again. This is going to be a monster migraine, I won't get any work done, and my whole week is ruined." This thought spiral triggers genuine anxiety and stress, which makes your muscles clench and, you guessed it, makes the headache even worse.
CBT gives you a practical framework to break that vicious cycle:
-
Awareness: First, you learn to catch those automatic negative thoughts in the act.
-
Challenge: Next, you start to question them. Is it really a guarantee your entire week is ruined? Have you ever managed a headache and still gotten things done?
-
Replacement: Finally, you consciously replace that catastrophic thought with a more balanced and realistic one. Something like, "Okay, a headache is starting. I have tools to manage this, and it will pass."
This isn't about slapping on a fake positive attitude. It’s about cultivating a more realistic and helpful inner voice. With practice, this mental retraining can genuinely reduce how intense and frequent your pain feels by stopping the stress response from pouring fuel on the fire.
"Mindfulness-based stress reduction and cognitive behavioural therapy have been shown to result in better psychological adjustment to pain and coping with it."
Calming the Nervous System with Relaxation Techniques
While CBT helps reshape your thoughts, relaxation techniques work directly on your body's physical reaction to pain and stress. When you're in pain, your sympathetic nervous system—the body's "fight or flight" alarm—is on high alert. This causes your heart to race, your breathing to become shallow, and your muscles to tighten, all of which can crank up the pain dial.
Relaxation techniques are the antidote. They activate your parasympathetic nervous system, which is your body’s "rest and digest" mode. This helps slam the brakes on the pain-stress cycle and brings back a sense of calm.
Practical Relaxation Skills to Try:
-
Deep Diaphragmatic Breathing: Forget shallow chest breathing. Focus on slow, deep breaths that come from your belly. Inhale through your nose for a count of four, feeling your abdomen expand, then exhale slowly through your mouth for a count of six. This simple exercise can quickly lower your heart rate and tell your brain it's safe to relax.
-
Mindfulness Meditation: This practice is about paying attention to the present moment without judging it. You might focus on your breath, the feeling of your feet on the floor, or the sounds in the room. This helps you create a bit of distance from the pain, allowing you to observe it as just a sensation, rather than getting completely swept away by it.
-
Gentle Movement: Activities like yoga and tai chi are fantastic because they blend gentle physical postures with focused breathing and mindfulness. They are brilliant for releasing stored muscle tension and quieting a busy mind. For a few ideas to get you started, you can explore these simple yoga poses to ease migraine pain and see what a difference it can make.
By making these mind-body techniques a regular part of your routine, you build resilience. You start to develop the skill of acknowledging pain without letting it control your entire experience, which gives you a real, profound sense of control over your own wellbeing.
Mastering the Everyday Pillars of Pain Control
While therapies and specific treatments are fantastic tools, the real foundation of managing pain day-to-day comes down to the habits you build. Think of sleep, nutrition, and how you manage your energy as the bedrock of your pain control plan. These aren't just quick fixes; they fundamentally change how resilient your body is to pain, giving you a powerful, proactive way to influence how you feel.
The link between these habits and pain is profound, yet it's often overlooked in conventional medical settings. Here in Australia, getting foundational support like nutrition or sleep advice isn't always part of the standard pain management conversation. In fact, one eye-opening study found that only 7% of consumers reported receiving nutrition support for their pain, and incredibly, none received interventions focused on improving sleep. This highlights a massive gap in holistic care. If you're interested, you can explore the findings of the CareTrack Australia study to see the full scope of this research.
This is exactly why taking charge of these pillars yourself is so critical. Let’s start with the most restorative habit of them all: sleep.
The Restorative Power of Quality Sleep
Sleep is when your body and brain get down to business with essential maintenance. It’s far from a passive state—it’s an active period of healing where inflammation is dampened, tissues are repaired, and the very pathways that process pain are reset. When you're running on empty from lack of sleep, your pain sensitivity can skyrocket, turning what might have been a minor ache into a major problem.
Even a single night of bad sleep can lower your pain threshold the next day. This kicks off a frustrating cycle: pain makes it hard to sleep, and the lack of sleep makes the pain feel so much worse. Breaking this cycle starts with improving your sleep hygiene—the environment you create and the habits you practice around bedtime.
Actionable Tips for Better Sleep Tonight:
-
Create a Sanctuary: Your bedroom should be your haven—cool, dark, and quiet. Blackout curtains can be a game-changer, and a white noise machine can help drown out disruptive sounds.
-
Stick to a Schedule: Try to go to bed and wake up around the same time every day, even on weekends. This consistency works wonders for reinforcing your body's natural sleep-wake rhythm.
-
Power Down Electronics: The blue light from phones, tablets, and computer screens tricks your brain into thinking it's still daytime. Make it a rule to put all devices away at least an hour before you plan to sleep.
Fuelling Your Body with an Anti-Inflammatory Diet
What you eat can either fan the flames of inflammation or help to calm them. An anti-inflammatory diet isn't about restriction; it's about consistently choosing whole, nutrient-rich foods that support your body's natural healing processes. This approach helps reduce systemic inflammation, a key driver behind many types of chronic pain.
Think of it this way: highly processed, sugary foods are like throwing dry kindling onto a fire, while anti-inflammatory foods are like gently dousing it with water. The goal is to gradually tip the balance in your favour.
Key foods to focus on include:
-
Fatty Fish: Salmon and mackerel are packed with omega-3 fatty acids.
-
Leafy Greens: Spinach and kale are antioxidant powerhouses.
-
Berries and Nuts: Blueberries, walnuts, and almonds all help fight inflammation.
By slowly bringing more of these foods into your meals while cutting back on processed snacks, sugary drinks, and refined carbs, you can make a real, noticeable difference in your pain levels over time.
The Art of Pacing Your Energy
For so many people living with chronic pain, life becomes a relentless "boom-and-bust" cycle. On a good day, you push yourself to catch up on everything you’ve missed, only to pay for it with days of agony and exhaustion. This is where pacing becomes an absolute game-changer.
Pacing is the art of balancing activity and rest to maintain a consistent energy level, preventing the overexertion that leads to pain flare-ups. It's about working smarter, not harder.
Imagine you have a daily budget of energy. Instead of spending it all in one go and going into "energy debt," pacing teaches you to spend it wisely throughout the day. This means breaking big tasks into smaller, more manageable chunks and scheduling short rest periods in between—even before you start to feel tired.
For example, instead of trying to clean the whole house in one frantic morning, you might clean just one room, then sit down and rest for 15 minutes. This simple shift helps you get things done without triggering a pain flare, giving you back control and preventing pain from dictating your life.
Exploring Evidence-Based Complementary Therapies
Once you’ve got the basics down, you can start exploring other powerful ways to manage pain without reaching for the pill bottle. A whole world of complementary therapies, backed by solid evidence, can offer significant relief. These aren't fringe ideas anymore; science is showing us exactly how they work with our body’s own systems to dial down pain.
Let's dive into two of the most well-regarded methods: acupuncture and TENS therapy. Both work in fascinating ways, tapping into the nervous system to either block pain messages or prompt your body to release its own natural painkillers. Think of it as working with your body's internal wiring, not against it.
Demystifying Acupuncture
Acupuncture might seem mysterious, but its roots in traditional Chinese medicine are now being explained by modern science. The practice involves inserting incredibly fine needles into specific points on the body. Traditionally, this was thought to correct imbalances in the body's energy flow, or 'qi'.
Today, we have a more scientific take on it. When the needles are inserted, they stimulate nerves, muscles, and connective tissue. This little nudge is believed to kickstart the production of your body’s own painkillers, especially endorphins. It’s like flipping a switch that tells your brain to release its most potent, built-in pain relief.
Because of this, acupuncture is a fantastic option for dealing with:
-
Chronic lower back pain
-
Neck tension and the headaches that come with it
-
Discomfort from osteoarthritis
-
Migraines
Interrupting Pain Signals with TENS Therapy
Another brilliant tool in the non-drug toolkit is Transcutaneous Electrical Nerve Stimulation, or TENS therapy. It sounds complicated, but it’s actually a small, portable, battery-powered device that sends a mild electrical current to your skin through sticky electrode pads. The sensation is usually just a gentle tingling or buzzing—nothing to be afraid of.
TENS works based on something called the ‘gate control theory’ of pain. Imagine the nerve pathways sending pain signals to your brain are like a single-lane road with a gate. When a headache flares up, that pain signal travels down the road, the gate opens, and you feel the ouch.
A TENS unit cleverly creates a bit of a 'traffic jam' on that road. Its gentle electrical impulses travel along the same nerve pathway, flooding it with non-painful sensations. This sensory overload effectively closes the gate, blocking the original pain signal from getting through to your brain. You aren’t fixing the source of the pain, but you’re successfully interrupting the message. And, much like acupuncture, TENS can also encourage your body to release more endorphins.
Just as TENS interrupts pain signals, other sensory inputs like aromatherapy can also influence our perception of discomfort. If you're looking for more ways to build your toolkit, you can learn more about natural headache relief with essential oils to complement these therapies.
Comparing Acupuncture and TENS Therapy
While both acupuncture and TENS are great for pain relief, they aren’t interchangeable. Knowing how they differ can help you have a more productive chat with your doctor or physio about which one might be a better fit for you.
Here's a quick look at how they stack up.
| Feature | Acupuncture | TENS Therapy |
|---|---|---|
| Method | Thin needles are inserted at specific points by a trained practitioner. | A mild electrical current is delivered via electrode pads on the skin. |
| Primary Mechanism | Stimulates nerves to release natural endorphins and other pain-relieving chemicals. | 'Closes the gate' on pain signals and can also trigger endorphin release. |
| Best For | Chronic, deep-seated pain; conditions like osteoarthritis, fibromyalgia, and migraines. | Acute and chronic pain; muscle soreness, nerve pain, labour pain, and post-operative pain. |
| Setting | Requires appointments with a licensed acupuncturist in a clinical setting. | Can be used at home with a portable, user-operated device after initial guidance. |
Ultimately, choosing between these therapies isn't about finding the one that’s "better." It's about finding the right tool for your specific pain and your lifestyle.
The goal is to feel empowered and take an active role in your own relief, and both of these methods offer a fantastic way to do just that.
Building Your At-Home Pain Relief Toolkit
Knowing about different therapies is one thing, but putting that knowledge into practice the moment pain hits is another entirely. This is where having your own ‘acute pain toolkit’ comes in—a curated collection of items and strategies you can reach for without a second thought. Instead of scrambling when a headache starts, you’ll have a plan ready to go.
This simple shift in thinking turns pain management from an abstract idea into a concrete, in-the-moment solution. Your toolkit doesn't need to be fancy or expensive; it just needs a few reliable options that give you a sense of comfort and control when you need it most.

Combining Proven Methods Into Modern Tools
A smart toolkit often includes items that cleverly bundle proven methods into a single, easy-to-use product. The Headache Cap, for instance, is a perfect example of this. It takes two of the most effective physical therapies for headache relief—cold therapy and gentle compression—and combines them into one wearable solution.
It’s about more than just convenience; it’s about making relief truly accessible. The hands-free design means you can get targeted cold and pressure exactly where you need it, without fumbling with a dripping ice pack and a towel. You can retreat to a quiet room, lie down, or even move around gently, all while managing your pain without putting your life on hold.
Your toolkit should be designed to support you, not create more work. Effective tools integrate seamlessly into your life, making consistent self-care feel effortless and achievable.
This modern approach simplifies how you respond to pain, making sure you get the biggest benefit with the least amount of fuss.
Integrating Your Toolkit for Maximum Impact
It’s crucial to see tools like the Headache Cap as one part of a bigger picture, not a magic bullet. They are most powerful when they work alongside the other non-pharmaceutical techniques you’re using.
Think of it like building a layered defence against pain. You might slip on your Headache Cap to get that immediate cooling sensation while also practising a calming mind-body technique.
Here’s a simple way this could look in practice:
-
Layer 1: The Physical Tool. You put on the Headache Cap to help numb the sharpest sensations and reduce inflammation.
-
Layer 2: The Mind-Body Technique. With the cap on, you start some deep, diaphragmatic breathing to help calm your nervous system’s fight-or-flight response.
-
Layer 3: The Environmental Support. You do all this while resting in a quiet, dimly lit room to minimise sensory input that can make headaches worse.
By stacking these elements, you’re hitting the pain from multiple angles at once. This integrated strategy is really the key to building an effective at-home toolkit and finding a reliable path to relief.
Got Questions About Drug-Free Pain Relief? We've Got Answers
It’s completely normal to have questions when you start exploring pain relief without reaching for the medicine cabinet. Moving beyond a medication-first mindset involves a bit of a shift, and it helps to have a clear picture of what to expect. Let's tackle some of the most common queries to help you feel confident.
A big one we hear is: do these methods actually work? The short answer is a resounding yes. Techniques like physiotherapy, CBT, and even something as simple as a hot or cold pack are supported by a mountain of evidence. They don't just put a band-aid on the pain; they get to the heart of the matter, addressing things like inflammation, muscle tension, or the thought patterns that can crank up your pain levels.
Naturally, safety is also a top concern. The good news is that most non-pharmaceutical options have an excellent safety profile, particularly when you compare them to the long-term use of certain medications. The key is to work with qualified professionals—like a registered physiotherapist or a licensed acupuncturist—to make sure you’re using the right techniques for your specific needs.
Can I Use These Methods Alongside My Current Treatment?
Absolutely. In fact, that's often the best way to do it.
Adopting drug-free pain management isn't about throwing out conventional medicine. Think of it more like adding new, powerful tools to your personal toolkit. These strategies can work hand-in-hand with treatments from your doctor, often helping to lessen your need for medication over time.
Just be sure to keep your GP in the loop. When everyone on your healthcare team is on the same page, you get a cohesive and supportive plan that’s built around you.
Why Is Everyone Talking About These Alternatives Now?
The growing focus on drug-free options stems from serious public health conversations. In Australia, the widespread use of opioids for chronic non-cancer pain, especially in rural and regional areas, has shone a spotlight on the risks of dependency and poor long-term outcomes. These areas often see higher prescribing rates due to a greater prevalence of chronic disease and limited access to other services.
You can learn more about the complexities of managing chronic pain in rural Australia to get the full picture.
This shift is all about empowering people with safer, more sustainable strategies that put you back in control, reducing the risks tied to long-term medication use.
Ready to add a powerful, drug-free tool to your pain relief toolkit? The Headache Cap combines the proven benefits of cold therapy and gentle compression into one easy-to-use solution for fast, effective relief. Explore the difference it can make at https://headachecap.com.au.





