A Guide to Trigger Points for Fibromyalgia
Living with fibromyalgia often feels like navigating a pain map that changes by the day. You know there’s a constant, dull ache—but not every sore spot is the same. Spotting the difference between fibromyalgia tender points and myofascial trigger points is your first step toward real relief.
Understanding Fibromyalgia Pain
Imagine your nervous system as a highly sensitive car alarm. Instead of only blaring during a break-in, it goes off at a gentle breeze or a passing cat. This overreaction is a simple way to see central sensitisation, where your brain and spinal cord dial up pain signals so you feel discomfort from things that shouldn’t normally hurt.
This heightened sensitivity underpins fibromyalgia, a condition affecting around 1 million Australians—roughly 3-5% of the population—with women diagnosed more often than men. Many people link its onset to significant stressors, whether physical trauma or emotional upheaval. For a deeper dive, visit Fibromyalgia Australia.
Tender Points Vs Trigger Points
Below is a quick comparison to help you immediately distinguish between fibromyalgia’s diagnostic tender points and the myofascial trigger points that send pain elsewhere.
“Tender points are indicators of widespread sensitivity, while trigger points are active sources of radiating pain you can often treat directly.”
Tender Points vs Trigger Points At a Glance
| Characteristic | Fibromyalgia Tender Points | Myofascial Trigger Points |
|---|---|---|
| Diagnostic Role | Localised soreness at 18 specific spots used by clinicians to confirm fibromyalgia | Tight, irritable knots in muscle that refer pain to other areas |
| Pain Pattern | Sharp tenderness confined to the exact spot | Radiating discomfort—like a knot in your shoulder causing a headache |
| Physical Feel | Similar to bruised spots; hurt when pressed | Firm bands or nodules within muscle tissue |
Understanding this distinction gives you a clear path forward. By targeting trigger points, you’re addressing the source of referred pain rather than just enduring its effects. This focus can be a game-changer in reclaiming your daily comfort and wellbeing.
Where to Find Common Fibromyalgia Trigger Points
Knowing what trigger points are is the first step. The real game-changer is learning to find them on your own body.
While these stubborn knots can pop up in any muscle, they have a few favourite hiding spots in people with fibromyalgia. This often creates confusing pain patterns that travel far from the actual source, making it a real challenge to figure out what’s really hurting.
This infographic gives a great visual of how the nervous system acts as the main hub, with tender points and trigger points being two very different expressions of pain branching off from it.
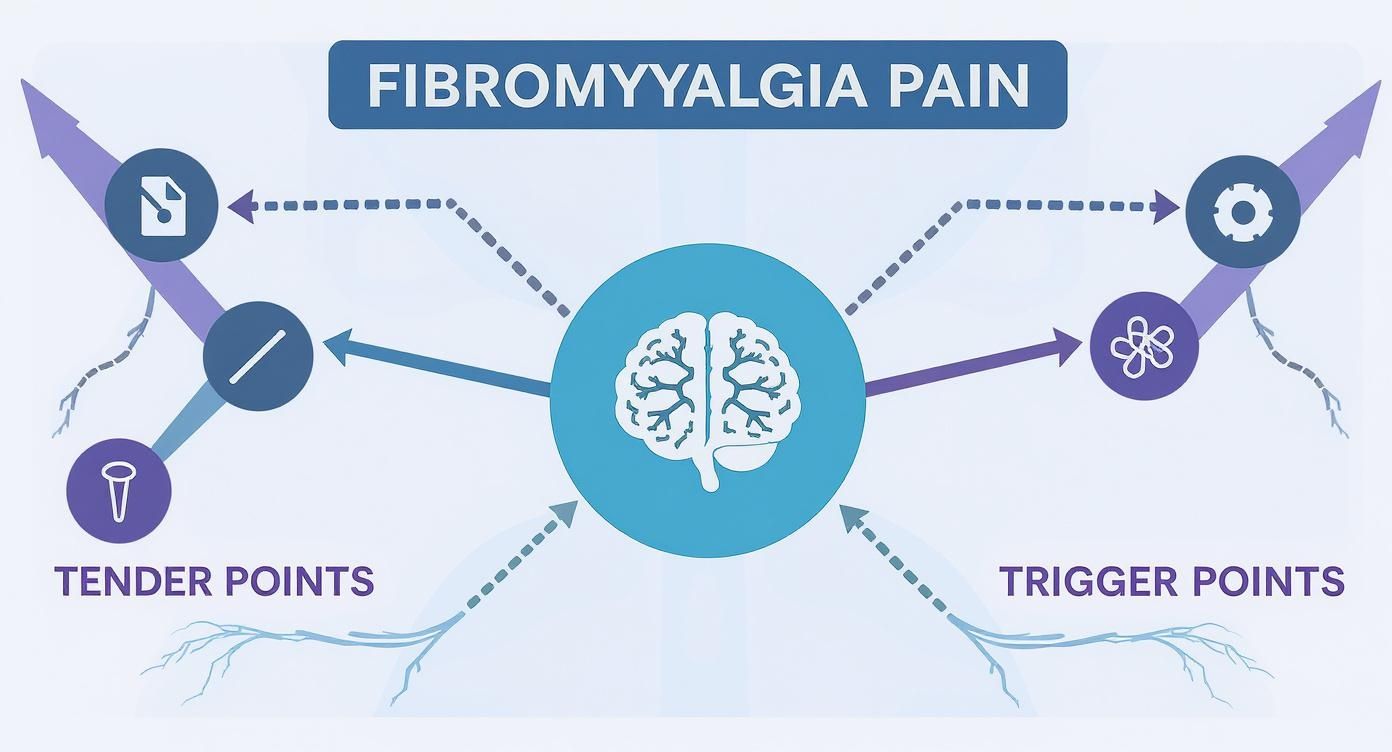
It’s a helpful reminder that even though both contribute to the fibromyalgia experience, they aren’t the same thing and need different approaches. Getting a handle on your trigger points can make a massive difference to your overall pain levels.
For many Australians, the onset of fibromyalgia can be traced back to a specific trigger. A study at a public hospital clinic in Australia discovered that 88.7% of patients could point to a distinct physical or psychological stressor that came just before their symptoms started. This really underscores how important it is to understand these pain patterns right from the beginning. You can read more about these findings and the diagnosis of fibromyalgia in Australia.
Neck and Shoulder Trigger Points
It’s no surprise that the neck and shoulders are prime real estate for trigger points. These muscles are constantly working to hold up your head, and they tend to soak up stress like a sponge.
- Trapezius Muscle: This is the big, diamond-shaped muscle covering your neck, shoulders, and upper back. Knots here are the classic culprit behind tension headaches, shooting pain up the back of your neck and into the base of your skull. Sometimes, the pain can even wrap around to feel like it’s behind your eye.
- Levator Scapulae: Running from the side of your neck down to your shoulder blade, a trigger point in this muscle causes that deep, nagging ache right in the corner of your neck. It’s the reason turning your head can feel so stiff and painful.
Upper and Lower Back Hotspots
Your back is a complex network of muscles supporting your entire upper body, which unfortunately makes it a magnet for these painful knots.
The biggest mistake people make is chasing the pain. With trigger points, the source of the problem is often somewhere else entirely. That persistent ache in your lower back? It could easily be coming from a tight knot in your glutes.
When these trigger points flare up, they can make simple things like bending over or even just sitting for a while feel excruciating. They’re a huge contributor to the widespread, achy pain that defines fibromyalgia.
Hips and Gluteal Muscles
The powerful muscles in your hips and glutes are often overlooked, but they’re notorious for developing trigger points that can impersonate other conditions.
- Gluteus Medius: This muscle is on the side of your hip. Trigger points here are masters of disguise, often causing pain that feels exactly like sciatica. You might feel it shooting down your leg or as a deep ache in your lower back and buttock.
- Piriformis: A small but mighty muscle located deep in the glutes. When it gets a trigger point, it can clamp down on the sciatic nerve, leading to pain, tingling, or numbness that travels down the back of your leg.
By patiently exploring these common zones, you can start to connect the dots between seemingly random aches and their true source. This gives you a personal roadmap to finding targeted, effective relief.
What Causes Trigger Points to Activate?
Trigger points don't just pop up out of the blue. They're a direct result of muscle stress and overload, which causes a small patch of muscle fibre to become a hyper-irritable, painful knot. Imagine a tiny, localised muscle cramp that just won't let go.
When you're living with fibromyalgia, your body is already in a state of heightened sensitivity. This means your muscles are much more prone to these kinds of stressors. So, factors that might be a minor annoyance for someone else can be more than enough to activate a trigger point if you have fibromyalgia. The nervous system’s habit of amplifying pain signals just pours fuel on the fire, creating a vicious cycle.
Common Activation Triggers
The reasons a trigger point suddenly "wakes up" are often tied directly to the day-to-day challenges of fibromyalgia. These factors can create the perfect storm for muscle tension and dysfunction, paving the way for these painful knots to form.
Key factors include:
- Chronic Stress: It's no secret that emotional and psychological stress makes us tense up. This isn't just a feeling; it causes muscles—especially in the neck and shoulders—to involuntarily contract for long stretches.
- Poor Sleep Quality: A lack of deep, restorative sleep means your muscles never get the chance to fully repair themselves overnight. This leaves them far more vulnerable to strain and injury the next day.
- Postural Strain: When you're in constant pain, your body naturally tries to protect itself. This often means hunching your shoulders or adopting other awkward postures that end up overloading specific muscles.
- Repetitive Motions: Even simple, repeated actions can be the culprit. Things you might not even think about, like typing or holding your phone, can strain muscle fibres over time.
Recognising an Active Trigger Point
Learning to spot the signs of an active trigger point is a game-changer for getting on top of the problem early. When a knot becomes active, the pain isn't always just in that one spot. It often broadcasts pain signals to other areas in a bizarre but predictable pattern known as referred pain.
A classic example of referred pain is a trigger point in your upper trapezius muscle (that big muscle between your neck and shoulder) causing a tension headache. The source of the pain is in your shoulder, but you feel it wrapped around your head.
You'll know a trigger point has flared up if you experience:
- A deep, persistent ache in a muscle that feels worse when you move.
- Pain that radiates to a seemingly unrelated part of the body. You can learn more about how neck and shoulder issues cause this kind of referred pain in our guide explaining why headaches happen.
- Increased muscle stiffness and a very noticeable loss of your normal range of motion.
- A palpable knot or tight, ropey band in the muscle that is incredibly tender when you press on it.
By becoming your own expert in spotting these signals, you can take action before the referred pain becomes overwhelming. It’s a powerful tool for managing your fibromyalgia symptoms and taking back control of your day.
Taking Control: Your At-Home Relief Toolkit

You don't always need a clinical appointment to manage the nagging ache of trigger points. In fact, learning a few safe and effective techniques to use at home can be incredibly empowering, giving you a greater sense of control over your day-to-day comfort.
The golden rule here is to be gentle and consistent. The aim is to gently persuade the muscle knot to release, not to strong-arm it into submission. Pushing too hard can easily lead to a painful flare-up, which is the last thing you want.
Gentle Self-Massage Techniques
One of the most immediate ways to tackle a trigger point is with gentle, sustained pressure. This helps break that exhausting pain-spasm cycle and encourages the knotted muscle fibres to finally relax. The best part? You don't need any fancy equipment—your own hands or even a simple tennis ball will work perfectly.
Here’s how to do it right:
- Find the Spot: Gently explore the sore muscle until you find that single point of maximum tenderness. That's the epicentre of the knot.
- Apply Gentle Pressure: Use your fingers, or pin a tennis ball between your back and a wall, to apply firm but gentle pressure directly onto that point.
- Hold and Breathe: Keep the pressure steady for 30-60 seconds. Focus on taking slow, deep breaths, and consciously try to relax into the pressure. You should feel the initial discomfort slowly start to fade as the knot gives way.
- Release Slowly: Don't just let go. Gradually ease off the pressure to give the muscle time to adjust.
A quick word of advice: you're aiming for a 'good pain'—that feeling of a satisfying release, not a sharp or worsening pain. If it feels too intense, ease off. Your body is your best guide, so listen to it.
The Power of Heat Therapy
There’s a reason a warm compress feels so good on a tight muscle. Applying warmth to these knotted areas can bring profound relief by boosting blood flow right where you need it. This increased circulation brings a fresh supply of oxygen to the distressed muscle, helps flush out the waste products that cause pain, and melts away stiffness.
This makes heat a fantastic first step before you try self-massage or stretching, as it helps the muscle become more pliable and ready to release. To get a better handle on the science, you can find out more about what heat therapy is and how it helps in our detailed guide.
Targeted Stretches for Common Hotspots
Once the muscle is warmed up, some gentle stretching can do wonders to lengthen those tight fibres and restore your range of motion. Just remember to focus on slow, controlled movements. Never bounce or push yourself past a point of mild, comfortable tension.
- For Neck and Shoulders: Gently tilt your head, bringing your ear towards your shoulder until you feel a light stretch along the side of your neck. Hold this for 20-30 seconds before slowly returning to the centre and repeating on the other side.
- For the Upper Back: Sit up straight and give yourself a hug, reaching your hands around to your shoulder blades. Gently round your upper back to deepen the stretch between your shoulders.
With stretching, consistency beats intensity every time. Just a few minutes each day can make a huge difference in easing the tension that allows trigger points to form in the first place.
Finding Professional Trigger Point Treatment

While at-home strategies are fantastic for day-to-day management, sometimes they just don't cut it for those really stubborn fibromyalgia trigger points. A huge part of any successful pain management plan is learning to listen to your body and knowing when it's time to call in the professionals.
So, when is that time? If you've been consistent with self-care but the pain just won't budge after a week or more, it's a clear sign. You should also seek expert help if the pain is severe, stops you from doing your daily activities, or if you start feeling other sensations like numbness or tingling. This helps rule out other underlying issues and ensures you get the right kind of care.
Clinical Treatments That Work
Here in Australia, we're fortunate to have access to several highly effective clinical treatments that can release trigger points and bring lasting relief. These are carried out by qualified practitioners who get the complexities of fibromyalgia and myofascial pain, so you know you're in safe hands.
-
Remedial Massage: This is a world away from a simple relaxation massage. A qualified remedial massage therapist has the skills to find and apply precise, sustained pressure to your trigger points. This manually breaks up the knotted muscle fibres and gets the blood flowing back into the area.
-
Dry Needling: Often performed by physiotherapists and other specially trained clinicians, this technique uses incredibly fine needles inserted directly into the trigger point. This causes a tiny 'local twitch response' in the muscle, which essentially forces the knot to release its tension and reset itself.
It's easy to confuse this with acupuncture. While both use needles, dry needling is grounded in Western anatomy and physiology. Its specific goal is to deactivate myofascial trigger points to ease pain and restore proper muscle function.
Choosing Your Path Forward
Trying to decide on the right treatment can feel a bit overwhelming, but you don't have to do it alone. Your GP or a good physiotherapist is the perfect starting point. They can properly diagnose what's going on and point you in the right direction.
When you go to your appointment, be ready to explain exactly where it hurts, what the pain feels like, and what self-care you've already tried. Giving them this detail allows them to build a treatment plan that's truly personalised to you, offering the best shot at real, long-term relief.
Your Questions, Answered
When you're trying to get a handle on fibromyalgia and its associated trigger points, a lot of questions pop up. Let's walk through some of the most common ones with clear, practical answers to help you better manage your pain.
Can I Get Rid of Fibromyalgia Trigger Points Forever?
This is the big question, isn't it? While you can definitely get those knots to release and "deactivate," the reality of living with a chronic condition like fibromyalgia is that they can come back. The best approach is to shift your goal from permanent eradication to consistent management.
Think of it like tending a garden. You can't just weed it once and expect them to never return. Through a steady routine of self-care and professional treatments, you can keep the "weeds" at bay, enjoy long periods of relief, and stop them from taking over your life.
How Do I Know If My Headache Is From a Neck Trigger Point?
A classic sign is a tension-type headache—that awful feeling of a tight band squeezing your head, or a dull ache that seems to crawl up from the base of your skull.
Here's a simple test: find one of those tight, sore spots in your neck or shoulder. Gently press on it. If doing that makes your headache flare up or reproduces that familiar ache, you've likely found the culprit. It's a textbook case of referred pain. Many people find relief by applying heat or cold directly to the neck; our guide explains how to find out if headache caps work for this specific type of pain.
Expert Tip: Trace the pain back to its source. A headache that kicks off with a stiff, sore neck is a massive clue that a trigger point is the real problem, not a primary headache issue.
Is It Safe to Massage a Very Painful Trigger Point?
You absolutely need to be careful here. The goal is to find what therapists call a "good pain"—a satisfying pressure that feels like it's doing something—not a sharp, make-you-wince kind of pain.
Start by applying gentle, steady pressure for about 30-60 seconds. Breathe deeply and try to relax into the pressure. You should feel the discomfort gradually start to fade as the knot releases. If the pain is sharp or gets worse, stop immediately. Being too aggressive can just irritate the area and trigger a flare-up. Always start gently and listen to your body.
For fast, drug-free relief from tension headaches caused by neck and shoulder trigger points, explore the Headache Cap range. Our reusable gel caps deliver targeted hot or cold therapy to soothe tight muscles and ease referred pain in minutes. Find your perfect fit and take control of your comfort today at https://headachecap.com.au.





