A Guide to the Face Pain Scale
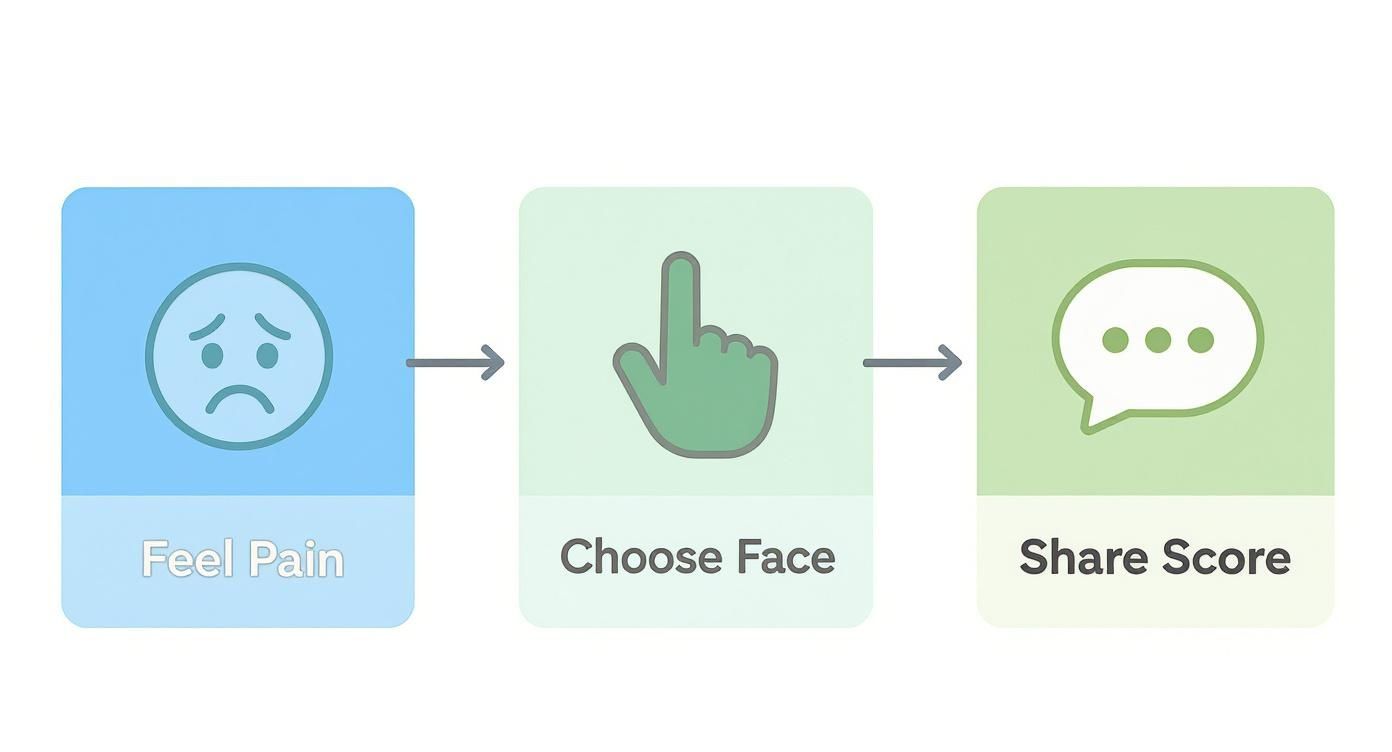
When you’re in pain, finding the right words to describe how you feel can be incredibly difficult. A face pain scale is a simple but incredibly effective tool designed to bridge that gap. It helps turn the deeply personal, subjective feeling of pain into a more objective score that everyone can understand.
A Universal Language for Pain
Trying to explain your pain can feel like describing a colour to someone who has never seen it. Is it a dull ache? A sharp, stabbing sensation? Words like "bad" or "awful" are vague and mean different things to different people.
This is precisely where a face pain scale comes in. By using a series of facial expressions or a simple numerical rating, it creates a universal language for discomfort. It helps translate your internal experience into a clear, standardised score that your doctor can immediately grasp, ensuring nothing gets lost in translation.
This shared understanding is the absolute foundation of effective pain management.
Why Measuring Pain Accurately is So Important
When your pain is measured consistently, it does more than just capture a single moment of discomfort—it tells a story over time. This data becomes a roadmap for your treatment journey.
- It Establishes a Baseline: Your first score gives your medical team a clear starting point. This benchmark is crucial for gauging progress later on.
- It Shows if Treatment is Working: By comparing your current pain score to your baseline, you and your doctor can see, in black and white, whether a new medication or therapy is making a difference. A falling score is a great sign, but if it stays the same or creeps up, it’s a clear signal to rethink the strategy.
- It Makes Communication Crystal Clear: There’s no ambiguity in a number. Saying your pain is a "7 out of 10" gives your doctor a much more precise picture than just saying it's "really bad." This clarity keeps everyone on your care team on the same page.
By turning a subjective feeling into objective data, a face pain scale puts power back into the hands of both patients and clinicians. It ensures that critical treatment decisions are driven by real information, not just guesswork.
Ultimately, this simple tool helps create a reliable log of your pain experience. This record is invaluable for spotting patterns, identifying triggers, and finding the most direct path to relief. Without this common language, managing complex conditions like chronic facial pain or migraines is a much tougher battle. It all starts with clear communication.
Comparing Different Types of Pain Scales
Just as a mechanic needs more than one type of wrench, healthcare providers use several different tools to measure pain. Not all pain scales are created equal; each is designed to work best in specific situations and for different people.
Getting this right is crucial. Choosing the right scale ensures your pain is communicated as accurately as possible, which is the first step towards getting effective relief.
Think of it like choosing the right measuring cup for a recipe. A simple cup is perfect for flour, but you need a much more precise instrument for a tiny dash of vanilla extract. In the same way, the best pain scale depends on who is using it and the specific type of pain they're trying to describe.
Let's walk through some of the most common scales used to assess facial pain, from the simple visual aids you might recognise to more specialised tools for complex conditions.
The Wong-Baker FACES Pain Rating Scale
For many of us, the Wong-Baker FACES Pain Rating Scale is the one we picture first. It’s that simple, intuitive line of six faces, starting with a happy, smiling face for "no hurt" and progressing to a crying, distressed face for "hurts worst."
Its real power is its simplicity.
This design makes it an outstanding tool for children, older adults, or anyone who might find it hard to put a number on what they’re feeling. It was originally developed back in the 1980s for kids, but its effectiveness means it's now one of the most widely used pain tools in the world for people aged three and up.
You can even see it referenced in official guidelines, like the Australian Triage, Assessment and Management of Patients in the Emergency Department, which speaks volumes about its reliability in a clinical setting.
Numerical and Analogue Scales for Adults
While the FACES scale is great for getting a general read, adults often need tools that can capture more subtle shades of pain. This is where numerical scales come in. The two most common are the Numerical Rating Scale (NRS) and the Visual Analogue Scale (VAS).
-
Numerical Rating Scale (NRS): This is the one everyone knows: "On a scale of 0 to 10, what's your pain?" Here, 0 means absolutely no pain, and 10 is the worst pain you can possibly imagine. It’s fast, straightforward, and gives a clear number that’s easy to track over time.
-
Visual Analogue Scale (VAS): The VAS is a little more nuanced. It’s a 10-centimetre line with "no pain" written at one end and "worst pain imaginable" at the other. Instead of picking a whole number, you make a mark on the line wherever your pain sits. The clinician then measures the distance from the start to your mark, which might give a score of 6.5 or 7.2. It allows for that extra bit of precision.
These scales are designed to turn something deeply personal and subjective—your pain—into a more objective piece of data. While a "7" for you might feel different from a "7" for someone else, your "7" becomes a consistent benchmark. It gives you and your doctor a reliable way to see if a treatment is actually working.
Both the NRS and VAS are mainstays in clinics for tracking everything from post-injury pain to the ups and downs of a chronic condition.
Specialised Scales for Specific Conditions
But what happens when the pain is more complex than just its intensity? For some conditions, especially neurological ones, a general scale just doesn’t cut it. This is where specialised tools are invaluable.
A perfect example is the Barrow Neurological Institute (BNI) Pain Intensity Scale, which was created specifically for trigeminal neuralgia—a condition notorious for its sudden, excruciating facial pain.
The BNI scale is different because it connects the pain score to how much it interferes with daily life:
- BNI Score I: No pain from trigeminal neuralgia, no medication needed.
- BNI Score II: Occasional pain, but not bad enough to need medication.
- BNI Score III: Some pain, but it's kept under control with medication.
- BNI Score IV: Some pain, and medication isn't controlling it well enough.
- BNI Score V: The pain is so severe, or the medication side effects are so bad, that you can't do any of your usual activities.
This functional approach gives a much richer, more practical picture. It helps doctors understand if a treatment is just taking the edge off or if it’s genuinely giving someone their life back. It highlights that with complex facial pain, how you feel is just as important as how you function.
To help you see the differences at a glance, here’s a quick comparison of the scales we’ve discussed.
Comparison of Common Face Pain Scales
This table provides a side-by-side look at different pain scales, outlining their format, who they're best for, and their main advantages. It's a handy reference for understanding why your doctor might choose one over another.
| Scale Name | Format | Best Suited For | Primary Advantage |
|---|---|---|---|
| Wong-Baker FACES | 6 illustrated faces showing increasing distress | Children (age 3+), adults with communication difficulties, quick assessments | Highly intuitive and removes the need for numerical or verbal skills. |
| Numerical Rating Scale (NRS) | A verbal or written 0-10 scale | Most adults and older children who can quantify their pain | Simple, fast, and provides a clear number that is easy to record and track. |
| Visual Analogue Scale (VAS) | A 10 cm line where patients mark their pain level | Adults in clinical or research settings requiring more precise measurement | Allows for finer gradations of pain intensity (e.g., 6.5) than the NRS. |
| Barrow Neurological Institute (BNI) Scale | A 5-point scale linking pain to function and medication use | Patients with trigeminal neuralgia | Measures the real-world impact of pain on quality of life, not just intensity. |
Ultimately, choosing the right scale is a critical first step. It's the foundation for clear communication between you and your healthcare team, which leads to better, more effective relief.
How to Use a Face Pain Scale Effectively
A face pain scale is so much more than just a chart of numbers or smiley faces. Think of it as a translator—a crucial tool that bridges the gap between the pain you feel and your ability to describe it clearly to someone else. Getting the hang of using it empowers both you and your doctor to work together on finding real relief.

Whether you’re the one in pain or you’re caring for someone who is, the objective is the same: to build a clear, consistent picture of the pain journey. This record becomes the bedrock for every decision that follows, from tweaking a prescription to trying a new therapy.
Guidance for Patients
When you're in the middle of a bad headache or facial pain flare-up, trying to pin it down to a single number can feel almost impossible. But here's the secret: consistency matters more than perfection. The goal is to give a reliable snapshot of what you're feeling in that moment.
Try not to overthink it. A quick, gut-feeling assessment is often the most accurate. If you’re torn between a 4 and a 6, just go with what feels closest. What’s truly valuable to your doctor is the pattern that emerges over days and weeks, not one single score.
To really make the pain scale work for you, try these simple steps:
- Create a Routine: Check in with your pain at the same times each day—maybe when you first wake up and again before bed. This helps establish a predictable baseline.
- Track Before and After Treatment: This is where the scale becomes a powerhouse. Note your pain level before you take medication or use a therapy. Then, check in again 30–60 minutes later. Did the score drop? By how much? This gives you solid proof of what’s working.
- Give Your Doctor Specifics: Instead of saying, “My headache got a bit better,” you can say, “My pain started at an 8, but after using my Headache Cap for 20 minutes, it dropped to a 4.” That’s precise, actionable information.
For example, if you're using something like a gel cap for cold therapy, tracking your pain scores before and after you put it on can be incredibly revealing. You can learn more about how to use a Headache Relief Cap here: https://headachecap.com.au/pages/how-to-use-headache-relief-cap. This simple tracking method can highlight just how effective it is for your specific pain.
Guidance for Clinicians and Carers
For healthcare professionals and caregivers, a face pain scale is an essential instrument for monitoring and fine-tuning a care plan. A series of scores tells a much richer story than a single data point ever could, uncovering patterns and responses that might otherwise go unnoticed.
Imagine each pain score as a dot on a graph. One dot doesn’t tell you much. But a line of dots reveals a clear trajectory—is the pain improving, stagnating, or getting worse over time?
A consistent record of pain scores transforms subjective feelings into objective data, allowing for more informed and responsive clinical decisions. It’s the difference between navigating with a compass and navigating with a detailed map.
To use the scale effectively in a clinical or care setting, keep these points in mind:
- Establish a Clear Baseline: That very first pain score is your starting line. Every score that follows will be measured against it to see if your interventions are actually making a difference.
- Look for Trends, Not Just Numbers: Is the patient's average pain score trending down week by week? Are the intense pain spikes becoming less frequent? These trends are what truly signal the success of a treatment strategy.
- Use Scores to Guide Adjustments: If a patient consistently reports their pain as a 7 out of 10 despite treatment, that’s a clear red flag that the current plan isn't cutting it. This data gives you the evidence needed to confidently recommend a change in medication, therapy, or dosage.
Ultimately, using a face pain scale is a team effort. It helps patients put their experience into words with clarity and gives clinicians the concrete data needed to provide the best possible care, leading to more personalised and effective pain relief.
Interpreting Pain Beyond the Scale
A face pain scale is a brilliant tool, but it relies on one simple thing: a person’s ability to point to a face or say a number. What happens when your patient is an infant, an older person with advanced dementia, or someone who simply can't speak? This is where we shift from asking about pain to seeing it.

Skilled observation becomes our most powerful diagnostic tool. A person's face often tells the story their words can't, offering objective clues that can guide compassionate and effective care. Learning to read this non-verbal language is just as important as understanding a pain score.
Decoding Facial Expressions
The human face is incredibly expressive. When we’re in pain, certain involuntary muscle movements are strongly linked to that discomfort. These aren't just random grimaces; they are specific, measurable actions that researchers have carefully categorised. By learning to spot them, caregivers and clinicians can make a far more accurate assessment of what someone is feeling.
Here are some of the key facial indicators to watch for:
- Furrowed Brow: The muscles between the eyebrows pull together, creating deep vertical lines.
- Tightened Eyelids: The eyes might be squeezed shut or squinted, almost as if trying to block out the sensation of pain.
- Wrinkled Nose: The nose often scrunches up, sometimes pulling the upper lip slightly higher.
- Raised Cheeks: The muscles around the cheeks tighten and push upwards.
- Opened Mouth: The mouth may fall open, often taking on a squarish, tense shape.
These aren't just subjective observations; they form the basis of clinical systems used to assess pain objectively. For instance, studies looking at intense pain have identified the most common facial actions. During severe pain episodes, eyelid tightening was the most frequent expression at 48.6%, followed closely by closing eyes at 42.9% and cheek raising at 42.1%. You can discover more insights about facial pain expression research on Frontiers.
When a person cannot speak, their face becomes their voice. Learning to listen with your eyes is a fundamental part of providing effective care, ensuring that even the most vulnerable individuals are seen and understood.
Context is Key for Accurate Interpretation
While these facial cues are powerful signs, they don’t exist in a vacuum. A furrowed brow could also mean deep concentration or confusion. That’s why a holistic approach is absolutely essential to correctly interpret what you're seeing.
To build a complete picture, you have to look beyond the face and consider other behavioural signs. These non-facial clues provide the crucial context that can confirm or challenge your initial observation. This is especially helpful when managing conditions involving referred pain, like identifying the complex trigger points for fibromyalgia, which can show up in unexpected ways.
When assessing a non-communicative person, look for these additional signs:
- Body Language: Are they restless and fidgety, or are they guarding a particular part of their body? Look for tense limbs or clenched fists.
- Vocalisations: Listen for moans, groans, whimpers, or crying. Any sound that’s out of character can be a sign of distress.
- Changes in Routine: Have they stopped eating? Are they refusing to take part in activities they normally enjoy? A change in sleep patterns is another major red flag.
By combining the observation of specific facial movements with these broader behavioural changes, you can piece together a much more reliable assessment of their pain. It ensures that even when a standard face pain scale isn't an option, you can still step in with the right support and make sure no one suffers in silence.
Practical Ways to Track Your Pain Over Time
Think of managing pain like being a detective. A single clue is helpful, but a detailed file of evidence is what cracks the case. While a one-off pain score gives you a snapshot, tracking your pain over time tells the complete story. When you consistently monitor your symptoms, you start to see the bigger picture—uncovering patterns, spotting triggers, and getting real proof of which treatments are actually making a difference.
This kind of detailed record is gold for both you and your doctor. You’re essentially building a comprehensive profile of your pain, and the more evidence you gather, the more precise and effective your treatment plan will be.
Keeping a Pain Diary
One of the simplest and most powerful tools you have is a pain diary. It doesn’t have to be fancy; a simple notebook or a note-taking app on your phone works perfectly. The key is to capture more than just a number on a face pain scale.
A truly useful pain diary entry paints a full picture of what you were experiencing. Make sure to jot down these key details:
- Date and Time: Pinpointing the exact time helps reveal patterns. Are your headaches worse in the morning? Does facial pain flare up after lunch?
- Pain Score: Use your preferred scale (like the NRS 0-10 or Wong-Baker FACES) to rate the pain's intensity.
- Pain Duration: Note how long it lasted. Was it a sharp, fleeting jab that was over in a minute, or a dull, constant ache that dragged on for hours?
- Potential Triggers: What were you doing right before it started? Think about foods, stress, specific activities, or even the weather.
- Relief Measures: Write down everything you did to get relief. Did you take medication? Use a cold pack like a Headache Cap? Rest in a dark, quiet room? Crucially, note what worked and by how much.
Recording this information helps you connect the dots between your daily life and your pain, putting you in the driver's seat of your own management plan.
Example Diary Entry
Sometimes, seeing an example makes it all click. Here’s what a detailed entry for a tension headache might look like:
Date: 25 October 2024
Time: 3:15 PM
Pain Score (0-10): Started as a 4, crept up to a 6.
Description: A dull, tight band of pressure right across my forehead and at my temples. Felt like a clamp.
Potential Trigger: A really long, stressful meeting at work with tons of screen time. I also skipped lunch.
Relief Measures:
- 3:30 PM: Took two paracetamol tablets.
- 3:45 PM: Grabbed my Headache Cap from the freezer and wore it for 20 minutes.
- 4:15 PM: Pain is now down to a 2. The cold therapy from the cap gave the fastest, most noticeable relief.
See the difference? This entry tells a story. It flags potential triggers like stress, screens, and hunger, and it clearly shows that cold therapy was a winner. Over weeks or months, these little stories build a powerful dataset for you and your clinician to work with.
Using Technology to Your Advantage
If a physical notebook feels like a chore, there are dozens of smartphone apps designed for tracking pain and other symptoms. Many of them can automatically log the date and time, ping you with reminders, and even create charts and graphs to help you visualise your pain trends over time.
Whether you go old-school with a diary or high-tech with an app, the secret ingredient is consistency. Diligent record-keeping helps you understand your own body better and gives your doctor the clear, specific details they need to fine-tune your treatment. It's also a fantastic way to measure the impact of non-pharmaceutical pain management strategies. A detailed log can provide solid proof of how much things like heat or cold therapy are improving your day-to-day life, backing a more holistic approach to your wellbeing.
Why You Can Trust These Simple Faces
It’s completely understandable to look at a simple drawing of a crying face and think, "How scientific can this really be?" But behind a tool like the Faces Pain Scale-Revised (FPS-R) is a surprising amount of rigorous medical science. These aren't just doodles; they're carefully designed and tested instruments, just like any other tool in a doctor's kit.
That rigorous testing is what builds trust. It gives patients, parents, and carers confidence that when you point to a face, you’re communicating real, credible information about your pain. These scales are trusted in hospitals worldwide because they consistently work, time and time again, across different ages, cultures, and medical conditions.
Making Science Accessible
Before any pain scale makes it into a clinic, it has to go through a strict validation process. Essentially, researchers have to prove that it actually measures what it says it measures—in this case, pain intensity. They do this by putting it to the test, comparing its results against other well-established pain scales in carefully controlled studies.
The goal isn't a matter of opinion. It's about establishing hard data to show the tool is consistent, accurate, and repeatable. When we understand the science behind them, it becomes clear that pointing to a face is a valid and vital part of assessing pain.
For example, a key study validating the FPS-R involved children aged five to twelve who were getting their ears pierced—a controlled, predictable source of pain. The results were striking. The FPS-R scores showed a strong positive correlation of 0.93 with another trusted measure, the visual analogue scale. If you're interested in the details, you can read the full research about these clinical trials.
This is the kind of solid evidence that proves the scale gives a reliable snapshot of a person's pain, regardless of their age or ability to find the right words.
Proven in Real-World Scenarios
A tool can work perfectly in a quiet lab, but the real test is a busy hospital ward. The validation for the FPS-R didn't stop with that first study. Researchers also tested it with hospitalised children who were in genuine pain from various surgical and medical conditions.
Even in that chaotic clinical environment, they found no significant differences between the scores from the FPS-R and other trusted scales. It worked just as well in the real world.
This proves that the simple faces hold up under pressure. They are not just pictures; they are scientifically sound instruments for communication, bridging the gap when words fail.
Ultimately, this mountain of evidence is why a doctor or nurse can confidently trust the information you give them using a face pain scale. It lets them make critical decisions about your treatment, knowing that your input is built on a solid scientific foundation.
Your Questions About Face Pain Scales Answered
It’s completely normal to have questions when you first start using a pain scale. After all, figuring out how to turn a complex feeling like pain into a simple number or a facial expression can feel a bit strange. But getting comfortable with these tools is one of the best things you can do to communicate clearly with your doctor and take control of your treatment.
Let’s walk through some of the questions that come up most often when people start tracking their pain.
How Often Should I Be Rating My Pain?
There’s no single, universal rule here – it really depends on what you and your doctor are trying to track.
If you're dealing with acute pain, maybe after dental work or a minor injury, your healthcare team might ask you to log your pain every few hours. This gives them a real-time picture of your recovery and helps them know if your pain relief is working. But for chronic conditions, like trigeminal neuralgia or persistent migraines, checking in once or twice a day is usually enough to spot meaningful patterns without it becoming overwhelming.
A good rule of thumb is to always log your pain during a bad flare-up or right after you’ve tried a new treatment, like using a cold therapy cap. That immediate feedback is gold. Most importantly, always follow the specific advice your doctor gives you.
What if My Pain Feels Like It's Between Two Faces?
This happens all the time. Pain isn't black and white, and it often doesn't fit perfectly into one of the neat boxes or cartoon faces on a chart. You might feel you’re somewhere between the face that’s just a little bit sad and the one that’s fully crying.
Don't get bogged down trying to find the "perfect" score. The goal here is consistency.
The real power of a pain scale isn't in one single, flawless rating. It's in the trend you see over days and weeks. If you decide to always round up when you're unsure, that’s perfectly fine – just stick with that method.
Simply pick the face or number that feels like the closest fit. Your doctor is looking for the overall pattern, not arguing over a 4 versus a 5.
Can These Scales Measure My Emotional Pain Too?
That's a great question, and it highlights an important distinction. Face pain scales were designed and tested specifically to measure physical pain – that is, sensations like throbbing, stabbing, aching, or burning.
While it's true that chronic pain can take a huge emotional toll, and a child might point to a sad face to express general unhappiness, these scales aren't built to measure psychological distress. For that, mental health professionals use different, specialised assessments to get a more accurate picture of what's going on emotionally.
At What Point Should My Pain Score Send Me to a Doctor?
Knowing when to pick up the phone and make an appointment is crucial. As a general guide, you should always seek medical advice for any facial pain that is new, severe (think a 7 or higher on a 10-point scale), or simply won't go away.
You should also see your doctor if your pain seems to be getting worse over time, isn't improving with standard over-the-counter pain relief, or comes with other worrying symptoms. Key red flags to watch for include fever, numbness, sudden weakness in your facial muscles, or any changes to your vision. Don't wait on those – get them checked out.
For fast, drug-free relief from headaches and facial pain, explore the options from Headache Cap. Find the perfect hot or cold therapy solution to soothe your discomfort at https://headachecap.com.au.





